Dr. Terry Hamblin has just made two posts to his blog under that title that shed some light on the question. They offer some additional perspective for those of you who have read my discussion Outwitting the dragon: Playing the treatment game.
Hamblin’s posts are worth a read. Among other things he discusses how the medical establishment has approached CLL by way of the more aggressive treatments needed for acute leukemia.
“Most doctors who design clinical trials for CLL have trained as acute leukemia doctors,” Hamblin writes. “Faced with a disease that may span decades they revert to type. Pharmaceutical companies are not much interested in a clinical trial that may last 20 years -- their patents will have run out. Current clinical trials, by common consent, have abandoned overall survival as an end-point; instead they have adopted complete response rate and progression-free survival as surrogates.”
Hamblin goes on to explain the problems with this, that complete response rates and progression-free survival are in the eye of the beholder -- depending on the test used to measure them -- and do not necessarily correlate with overall survival. It’s all a rather messy business, where a certain degree of guesswork is inimical to the process.
So, what is the aim of treatment?
Hamblin leaves that question open, so I will throw in my two cents and provide the answer as I see it:
To maintain a good quality of life for the patient for as long as possible.
Notice I said “good quality of life.” There’s the rub. In a disease that is chronic, that may or may not progress very far, or that may progress rather slowly, what is the point of treatment that might reduce the quality of life?
In fact, maintaining a good quality of life for as long as possible may also involve not treating or treating less.
Treatment of CLL is seldom a necessity if one defines “need” as something that has to be done or the patient may soon die without it. CLL patients do not die of high lymphocyte counts. Most often they die of infections that their compromised immune systems are no longer able to fight off. From what I’ve read, this seems to result from two things:
One, in end-stage CLL, the mutant B cells can so completely infiltrate the marrow that other cells, such as infection-fighting neutrophils (not to mention red blood cells and platelets) can no longer be produced. Or:
Two, complications from chemotherapy, which involve collateral damage to the immune system, have left the body neutropenic, practically devoid of T cells, and unable to mount a defense against invaders.
It seems to me that number two is the cause of more problems for more patients than number one. If I had another day or two, I could list so many scary side effects from chemo that one might think that the very act of undergoing it is suicidal.
It is not, of course. Chemo has its place. It’s just that in CLL, when we are talkin
 g about overall survival and quality of life, that place may not be as front-and-center as it is with other cancers. Doctors trained to fight cancer -- not just acute leukemia -- have a hard time with the concept of watching it spread. They revert to type.
g about overall survival and quality of life, that place may not be as front-and-center as it is with other cancers. Doctors trained to fight cancer -- not just acute leukemia -- have a hard time with the concept of watching it spread. They revert to type.Complications from chemo can also have the unintended effect of ramping up the disease, making it resistant to many therapies, by selecting for treatment-resistant CLL clones. If you get a remission that lasts three years and have burned most of your bridges, what is the point? Unless there is a pressing medical necessity, why not wait out those three years, or as many of them as you can, and then start treatment? (Sorry, vanity is not an excuse. None of us wants to look like a chipmunk, but I’d rather be a living chipmunk than a dead Adonis.)
So when I look at the question of when to treat and with what -- which is an enormously important part of the equation -- what are the factors that it boils down to in my mind? And what have I come to regard as a “pressing medical necessity?”
Obviously there are different factors at work in different people. (People with aggressive CLL have a whole ‘nother can of worms to consider and should probably ignore much of what I’m saying.) I can only speak for myself. But here is how I look at it:
So far my body has managed to cope with CLL for what I believe has been at least ten years. The rest of my immune system is weakened but still more or less functional. Typhoid Charlene came to visit and I was the last to get her cold and the first to get over it. My neutrophils are always in the normal range, even after treatment with Rituxan. There is no point yet in throwing my immune system for such a loop that it becomes almost completely useless.
So what would make me think that it's time to risk a little loopiness? Well, any one of the following:
1. If my platelets were trending downward and dropped to a point --and stayed there -- that I would be unable to clot blood and might suffer a severe hemorrhage. Say around 40.
2. If my hemoglobin (HGB) dropped to the point that I started suffering from anemia, leaving me weak and tired and left with a diminished quality of life.
3. If my liver function were seriously compromised, or if the CLL was having some other unusual or rare effect -- paraneoplastic pemphigus on the skin, for example -- that it might lead to a debilitating or life-threatening second condition. Hamblin points out that CLL cells migrate throughout the body, even into the brain, and one never quite knows what will happen when they take up residence somewhere. The "monkey wrench" factor is part of living with the disease.
4. If the disease began to take a more aggressive course, showing a sudden ramping up of symptoms, perhaps caused by a clonal evolution, that became noticeable in rapid lymphocyte doubling time or dramatic increase in lymph node size.
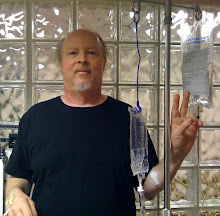
As many of you know, I have already been treated three separate times with Rituxan. My doctor and I are making the calculated guess that this mild treatment will keep the disease under enough control that I can continue to live with a good quality of life. So far this has worked, normalizing (or close) the lymphocyte count in the blood, reducing many nodes, keeping the spleen in check, bumping up my platelets during treatment, and hopefully keeping errant colonies of CLL cells from getting into too much mischief elsewhere.Were I to leave the disease uncontrolled, I believe the day would arrive sooner rather than later when mild treatments alone might not suffice. I am IgVH unmutated, and therefore the CLL reproduces faster. There is no doubt that the faster it reproduces, the more problems there will be.
But if Rituxan did not exist, I would not go in for treatment at this point.
The blunt fact is that chemotherapy is not curative, and that it inevitably, to one degree or another, has side effects that can and will diminish one’s quality of life. Even Rituxan is not risk-free, destroying as it does normal B cells as well as the mutant ones; this includes memory B cells forged from fighting previous invaders, which can play an important role in secondary immunity. It may also have a negative effect on immunoglobulins in some patients.
There is a Stage IV CLL patient who posts to an internet list on occasion. She had fludarabine, once, many years ago. She has now opted for what is called palliative care -- care designed to relieve symptoms rather than cure a disease -- and in her case, this means red blood cell transfusions. This has worked for her for two years, much to the amazement of her doctors. Her platelets are also below normal, but the numbers have bounced around and she has required no transfusions in that department. She has burned no bridges during this time and reports having a good quality of life. She is accomplishing precisely what I would define as the aim of treatment.
What is wrong with her approach? Nothing, other than that it flies in the face of conventional wisdom. But haven’t we all learned by now that CLL itself flies in the face of conventional wisdom? And that, short of a stem cell transplant, all therapy for CLL is -- guess what? -- "palliative"?
In my view, failing to recognize these facts gives birth to any number of dangerous assumptions and unnecessary, precipitous acts.





7 comments:
once again you have hit the nail the nail on the head with how I think. Keep up the good work. Elyse
David: your blog brings home the truth that nothing can substitute for common sense, specially when one's life hangs in the balance.
Science is indispensable to the understanding of the pros and cons but when it comes to making a value judgment, science has nothing to say, - that's something many patients (and many doctors as well) fail to grasp.
Thanks to all for your comments. Andy, I think you are exactly right in calling this an issue of common sense. I think we patients (and our doctors) can get so caught up in parsing the trees that we forget to look at the forest.
You dismiss those who seek treatment for 'chipmunk cheeks' as being pathetic vanity-philes.
You are way to harsh in your criticism, and you betray a lack of understanding some of the subtleties of the disease.
Grossly enlarged lymphnodes qualify as 'bulky disease', which is terribly difficult to treat effectively. You should know that.
You miss the mark here.
I'm not sure that the last poster understood what I was saying about the vanity issue. Vanity is not a reason to treat but I am aware of cases in which it has been used as a reason for treatment. The NCI guidelines call for treating when nodes reach 10 cm; in some cases that can be way too big for comfort and it is easier to treat nodes that are smaller than that, especially if one is using Rituxan alone.
Readers of this blog know that I have a very conservative approach to treatment but that I also think chemotherapy has its place when used at the proper time. I have also always said that I respect the decision each of us makes when it comes to treatment because I know how hard it is to reach that decision. We must all find the treatment we truly believe in, whatever it may be.
My oncologist has suggested taking both Rituximab and Fludarabine in order to suppress amyloid production (IGM lambda), which has been seen in my muscles and is causing Inclusion Body Myositis symptoms. It does seem highly likely that this regimen will suppress the amyloid and thus possibly help the muscles, and prevent amyloid accumulation elsewhere (and possible demise!). But is the "cure" possibly worse than the disease? Possible to simply take Rituximab? Or, do nothing at all?
I'm not familiar with the condition the last commenter describes. One question I would have is whether adding the fludarabine would alleviate the problem for good, or for a long, long time. Or would it be a short fix? You mention "possible demise," so I gather this is a potentially serious matter, not unlike my AIHA. I would seek a second opinion from an expert doctor, one familiar with your condition and its treatments. Perhaps there is a milder approach that will work; if not, I still would not hesitate to get the treatment I needed.
Post a Comment