That's tough stuff to hear. But these sorts of questions can weigh on the minds of CLL patients with progressing di
 sease, especially younger ones for whom the bell seems to toll all too soon. We are the rock and roll generation, after all: Live fast, die young.
sease, especially younger ones for whom the bell seems to toll all too soon. We are the rock and roll generation, after all: Live fast, die young.CLL affords its victims the grace of time -- time to say goodbye, to make amends, and to think about the consequences of fighting, and of not fighting. Those who had always hoped for a quick and painless passing may find this discomfiting. With CLL, one's passing might be relatively painless, but it is not quick.
And so it is legitimate to wonder about things that our friends and family would rather not hear. Some of you reading this are no doubt thinking "I wish Dave would write some more about his automated trash can." But death is potentially part of the CLL picture, and it is a fair topic of conversation.
And so I entered the discussion my friends were having, and this is what I said (with a little extra added in hindsight, as is a writer's prerogative, thus making me seem much more erudite than I did at the time):
There is a time to lay down one's arms, give up the fight, and go gently into that good night. This is when people quietly decide enough is enough and simply give themselves permission to let go, letting the end come when and how it may. Some go into hospice, some stay at home; I’d like to drag myself to the beach and stare at the sea and be carried away by its rhythm.
But for me, that time will not come until every avenue is exhausted. I have heard transplant stories, and transplants can be a living hell, but they can also be relatively easy. Even for people who have to put up with all kinds of problems, the benefits can outweigh the drawbacks. Patient blogs tell the story: A 17p-deleted patient on her second transplant who, despite skin problems, goes on a cruise. A young father, in his 40s, who suffers post-transplant seizures but finds them a small price to pay for the privilege of being here with his wife and kids.
So long as I can prop my ass up in bed, hold the hand of the woman I love, laugh at stupid puns, listen to music, see the hawks flying outside my window, taste a fresh apple, and smell the desert sage after a rain, I will fight this thing.
Why not do a transplant now, cut out all the intervening waiting and worrying and fighting that can drain you emotionally, financially, physically? Well, transplants are risky (even if they hold out the promise of a cure for some) and the longer I wait, the better the procedure will get. It's all a matter of timing. I'm 50. I can wait 10 years, if the disease will allow it, which it probably won't. But I can have a pretty good quality of life for the next however many years, and then roll the dice.
I am not a gambler but this disease is making me one. CLL is all about gambling. Dice. Poker. (Russian) Roulette. Pick your metaphor. Leukemia is filled with games of chance. Timing is everything, along with luck.
Sure, it's tempting to go with something like RFC to get a great remission now and not have to worry for awhile. But the cruelest thing about this disease is that these remissions don't last, and they get harder to duplicate. Is chemo a fool's paradise? Or does it allow for a last bit of real paradise (aka disease-free living) before the shit truly hits the fan? I can't fault anyone for going with chemo now; who knows how it will all turn out. The best we can do is play it as we see it.
Should we avoid a transplant, sit tight for as long as we can, and wait for a cure? (Calling Mr. Godot!) I don't think we'll see a cure anytime soon, especially for those of us who have gone beyond the infancy of the disease. Honestly, I think we're at least 20 years away from a cure. A CLL expert doctor once said that the fight against CLL will be one long war of attrition. I think he's right. What this means is that we patients have to play the game with the cards we're dealt today. (Who knows, maybe we can exchange a card or two
 if things go right; I don’t think a cure will come soon, but I do believe there will be incremental progress in treatment.) None of this is a reason not to stay in the game.
if things go right; I don’t think a cure will come soon, but I do believe there will be incremental progress in treatment.) None of this is a reason not to stay in the game. And so I say, hang on.
There will be plenty of time to explore the world after this one. So long as the sun rises and there is music to be made, so long as there are exotic ports of call and children to hug, this life grants enough small pleasures to make the pain of struggle worthwhile.
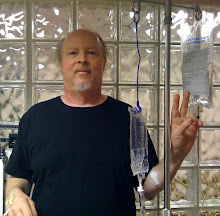
So, hang on. As long as Marilyn can hold my hand and I can know she's there, I'm going to hang on.
Today is our 24th anniversary. I do not know if there will be twenty-four more. But it won’t be for lack of trying. Happy anniversary, my sweet. Together, we will see what love can conquer.