Since my last post I've gotten some encouraging results from a PET/CT scan, and I've passed three dates of note on the calendar.
First, the PET/CT, which was done as I was finishing the fourth round of R-EPCH in early September. A PET/CT is how doctors keep track of the progress being made by DLBCL patients (remember, thanks to Richter's Transformation some of my CLL became Diffuse Large B Cell Lymphoma).
My first PET/CT in April, at diagnosis, was scary. It showed massive tumors, "too numerous to count," which lit up like a Christmas tree. When I say "lit up," I mean that the standard uptake value (SUV) of the radioactive glucose solution they put in my bloodstream was positive for aggressive lymphoma. (Oh how I wish I lived in a world where the only thing SUV meant to me was "sport utility vehicle")
The SUV of the tumors ranged from a high of 26.20 down to 14.03. By comparison, "background" SUV -- that of noncancerous normal tissues, is 2.5 in the liver and 1.5 to 2.0 in the mediastinal blood pool. Both are often used as comparison tools. According to one research paper:
a SUV ≥ 13 in the most intense lesion is highly indicative of
aggressive histology, while
a SUV ≤ 6 is much more compatible with indolent lymphoma, unless
the clinical course indicates otherwise
My September scan showed a marked reduction in swollen lymph nodes, with few remaining. And the SUV of the node under my left arm, for example, dropped from 17.2 in April to 1.1 in September. The largest nodal mass in my abdomen showed an SUV drop from 18.8 to 1.8 (and a drop in size from 25 x 25 cm in April to 13.4 x 9.2).In other words, my SUV was now at background levels. My oncologist, Dr. Droll, said, "If there were still high-grade lymphoma, it wouldn't look like this. . . . These things light up like CLL would light up."
Needless to say, Marilyn and I were quite happy with the report, which was better than we dared to hope.
Does that mean I'm lymphoma-free, back to plain old CLL, which is, I hate to say it, by comparison a "good" cancer, or at least much better-behaved?
Well, maybe. I have learned that a CR ("complete response") in DLBCL is very much like a CR in CLL: there may still be some cancer cells lurking around that still may cause a relapse, not all of which are detectable on even the most sophisticated test. As with CLL, clinical symptoms are the bottom line, and only time will tell if I relapse.
I still have some swollen nodes and an enlarged spleen. Maybe they're all filled with CLL, and maybe there are just a few really nasty lymphoma cells that have survived and are lurking in there somewhere.
Does my response to the chemo mean that I can put off having a transplant? Possibly. But there is still wisdom in considering the transplant option. CLL doesn't get better the longer you have it, and neither, I presume, does DLBCL. (As one lymphoma expert pointed out to me, the CLL could always transform again.) At the age of 57 I am still young enough to tolerate a transplant -- I have tolerated the chemo quite well -- but I won't be a picture of youth and vigor forever.
Further, to get me to this point I have undergone some heavy-duty chemo that I can't responsibly use again, even as transplant conditioning. Adriamycin is a drug that does wonders against lymphoma, and it is a component of both R-EPOCH and R-CHOP. It has also been implicated in congestive heart failure if you do too much of it, and if I were to do any more past Round 6 of R-EPCH, I would be doing too much.
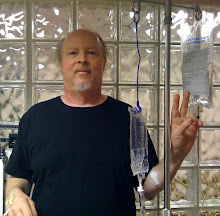
Speaking of chemo, it is the standard of care for DLBCL to go the distance, all six rounds, of R-EPCH, even if the PET/CT after the fourth shows no evidence of lymphoma. The theory is that the more chemo, the more undetectable stuff you kill, the better off you are. So I have now completed Round 5 and I'm scheduled to go back to the hospital for the final round next week.
We've spent more than 40 days in the hospital this year -- I say "we" because Marilyn comes with me and sleeps in a fold-out chair next to me; hospitals really need double beds. The chemo is given over five days, with a visit to the doctor's office for a Neulasta shot on the sixth.
The hospital staff -- the chemo nurses of Six South at Banner Baywood Medical Center in Mesa, AZ -- have been great; I spent my birthday in there during the last round, and they surprised me with a round of "Happy Birthday" and a gift. Food service even provided a small cake.
The birthday is one of the calendar dates I mentioned at the start of this post. Another is the September 3 anniversary of my CLL diagnosis -- my tenth anniversary, as it turns out. No singing, no cake, just an "ugh" in recognition of the event.
The last date of note was October 1, the opening of the Health Insurance Marketplace. Thanks to President Obama and the Democrats, I will be able to purchase health insurance that covers a transplant. My current health plan specifically prohibits it, and because of my preexisting conditions, no one else would insure me -- until now, when preexisting conditions cannot be held against you.
So, bottom line, the Affordable Care Act is potentially a matter of life and death for me. Thank you, Mr. President. May we, as a nation, always listen to the better angels of our nature.