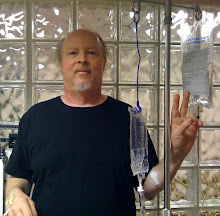
To guard against tumor lysis, my first treatment involved only two-thirds of the standard dose of bendamustine (aka Treanda); this time I had the full 100mg/m2. My reaction was significantly more intense than the easy-breezy first time around.
The bendamustine was administered last Tuesday and Wednesday. Tuesday also included the Rituxan, which brought forth infusion reactions unlike any I have had before. The ill effects of the bendamustine -- fatigue and low-level nausea -- didn't set in until Thursday night, and have only really abated today.
More on that later. First, there is good news to report. The higher dose has done a much more noticeable job on the nodes, almost returning my neck to its natural swanlike appearance, and reducing a large mass in the abdomen to a reasonable degree. I still have a long way to go with the nodes, but if this keeps up, I will have made significant progress by the time I'm through.
One question is how long the nodes will stay at their current size. Last time around, they began to bounce back in the week before my second treatment. By the time I sat down in the infusion chair, most of the progress that had been made thanks to the first round had been erased.
This is not a good sign, and it indicates how fast my disease is prone to grow. But my reaction to round two, with a much more noticeable node reduction than round one, makes me cautiously optimistic that the effort will hold this time. Which, fingers crossed, means round three should see an overall further reduction in the nodes.
I am hopeful that the cumulative effect of the treatments will largely shut down the CLL factory in the marrow as well as reducing it in the nodes, creating a smaller, more easily manageable disease.
A FISH story
For some time I have wondered if my disease has turned more aggressive, or whether it has reached a critical mass, like a snowball rolling downhill, gathering size until it gets so big that it is difficult to stop.
A first step was to get a new FISH test, which I did in April. Would there be a 17p deletion there, indicating more aggressive disease?
The results were a little surprising. My first FISH test, back in 2004, showed a "normal" karyotype, which meant the chromosomal damage was of a nature not probed for on the test. In 2006, the FISH came back positive for the 11q deletion on 24% of cells examined, not good news. 2007's FISH showed 11q in 36% of cells. 2008's FISH showed 11q on 53% of cells. In 2009, 11q was noted on 31% of cells examined. (Why the dip? Who knows? But it didn't change the basic picture: an 11q
deletion that appeared to have increased in the number of cells over
time. By the way, the deletion always showed up on one arm of the chromosome only, which was of some comfort, as it meant I still had some ATM function, ostensibly.)
2010 and 2011, the Revlimid years, were FISH-free as the disease was under control for most of the time. Then in April of this year came an interesting twist: the 11q was down to 8% and a new deletion, 13q, again on one arm of the chromosome, was found on 30% of cells examined.
That FISH test was from the peripheral blood. In July, I had a bone marrow biopsy, which showed 90% involvement by CLL. A FISH was performed on that sample. It showed no 11q deletion at all, and a 13q deletion on 42% of cells.
So, what does all this mean? It appears my 11q clones are in decline, which is good news. (Why that is, again, who knows? It appears to fly in the face of conventional wisdom. My hunch, which is a completely wild guess, is that my Revlimid treatments had something to do with it.)
The April FISH showed a double deletion (11q and 13q), which is not good news. And while 13q is considered the most benign of the deletions, there are a couple of flavors of 13q. One indicates more aggressive disease; the tests I had did not go beyond the basic probe, indicating a deletion of one arm of 13q14.3.
I don't think the handoff from 11q to 13q indicates an improvement in my disease. But this is about the best change I can hope for; it would seem to indicate that the disease is probably not more aggressive by nature than it was before.
So I am basically subscribing to the snowball theory, and only time will tell if I am right. Another point I am compelled to make: FISH tests are all well and good, but shy of showing a 17p deletion, the most important factor in deciding to treat the disease is your clinical condition.
On the way from Calais
The last time I recall feeling as nauseous as I did post-bendamustine was many years ago on a boat from France to England. This was in the pre-Chunnel days. I grew whiter and whiter as the white cliffs of Dover approached, barely managing to contain my nausea with each bumping wave.
The nausea that set in last Friday never got to the barfing point, but it was uncontrollable with ondansetron (Zofran) tablets, which worked less well than Pepto-Bismol. To keep my kidneys flushing the dead CLL cells through, I needed to be drinking lots of water, and water is the last thing a sensitive stomach can tolerate. If I never see another can of Blue Sky New Century Cola again, it will be too soon. Needless to say, food was also rather unwelcome; I managed to lose some noticeable weight since nothing was appealing, although my stomach eventually discovered that macaroni and cheese was tolerable.
The fatigue was also way out of the ordinary. I would sleep 14 hours, on and off, and wake up tired. Today, Wednesday, is the first day that feels normal, both in terms of fatigue and nausea.
Although it sometimes felt as if my hemoglobin had taken a hit -- benadamustine can lower hemoglobin temporarily in about 90% of cases -- it turned out that wasn't the case. Comparing some numbers from the day before I started the second round to six days after I finished it: hemoglobin 10.8 before, 10.5 after; platelets 147 before, 138 after; absolute neutrophils 4.9 before, 5.4 after (as in the first round, I had a Neulasta shot on the day after completing treatment). The only dramatic change was in absolute lymphoctye count: 13.6 before, 2.1 after. I don't think my ALC has ever been so low.
UPDATE: My blood work from two weeks after treatment showed signs of decline in hemoglobin (down to 9.3) and platelets (110). Absolute lymphocyte count was 1.4, a new record low.
UPDATE: My blood work from two weeks after treatment showed signs of decline in hemoglobin (down to 9.3) and platelets (110). Absolute lymphocyte count was 1.4, a new record low.
The rigors, minus the mortis
Last Tuesday's plan was to infuse the rituximab, then the bendamustine. My reaction to rituximab, a drug I have had countless times, was surprising. I was given prophylactic Benadryl and Solu-Medrol and expected pretty smooth sailing. About 15 minutes in, my face turned red and I felt some shortness of breath. This eventually abated, thanks to stopping the treatment, accompanied by some oxygen.
About 10 minutes after the infusion resumed, I experienced what the chemo nurses called "the rigors." This symptom was appropriately named, as it involved rigorous uncontrollable shaking. You can wear out your thigh muscles fast when this
happens. Imagine having "the chills" but it's all coming from an
internal place, so it doesn't matter how many blankets they pile on you,
you still can't get warm. I think the rigors lasted about 15 or 20 minutes, during
which time I found myself wondering whether this was what the passengers
on the Titanic went through when they fell into the icy Atlantic. It finally abated, thanks to some more Solu-Medrol and Benadryl, as well as some Demerol. The Rituxan was stopped and I was given the bendamustine; reversing the order sometimes helps in such cases. Sure enough, when the Rituxan infusion was resumed later, it was completed without incident.
Why would someone who had managed to accommodate Rituxan for years with minor reactions, if any, suddenly develop these sort of symptoms? Again, who knows? With groundless abandon, I theorize that Revlimid changed something in my immune function. The Revlimid put an end to my autoimmune hemolytic anemia, but also led to a more hair-trigger allergy response in terms of skin rashes. Perhaps it also created a microenvironment less friendly to Rituxan.
My next sojourn in the chair is scheduled for mid-September. Keeping my eyes on the prize, I look forward to making more progress against the disease. But I'm not counting on an easy ride, and I will lay in a supply of macaroni and cheese, just in case.