skip to main |
skip to sidebar
Imagine two oncologists starting a practice, then imagine the same two oncologists having a falling out two years later. Welcome to the Onco Wars, raging now at the office where I have been receiving care for my chronic lymphocytic leukemia.
I'll call them Dr. Belle and Dr. Tower. You can think of them as Godzilla vs. Megalon, with all the attendant fire-breathing and foot-stomping that entails.
On January 23, Dr. Belle, my doctor, wrote a letter to her patients:
"It is with sadness and a heavy heart that I announce that, due to unforeseen circumstances, I will no longer be able to attend to you as your physician. This letter is to advise you that I will not provide professional medical services to you after January 30, 2012. Your current condition requires follow up and I encourage you to find a new physician promptly to continue this care . . . I suggest you contact your insurance plan representative for assistance in locating a new hematologist/oncologist to assume your care . . ."
 And on January 27, Dr. Tower wrote to Dr. Belle's patients:
"Dr. Belle has recently informed us, and sent a letter to you, stating that she will be leaving the practice effective 1/30/12. Let me assure you that our office still remains committed to serving your needs and assisting in your care. I understand that Dr. Belle's departure may be upsetting to you, but I assure you that I am more than willing and able to assume your care, and would in fact be honored to do so . . ."
There is no doubt an interesting back-story here, which I don't imagine I will ever know. For me and for Dr. Belle's other patients, the big news is that we don't have a doctor anymore. Dr. Tower wants us to stay, but I hear through the grapevine that a number are choosing to go.
For me, all this comes at the worst possible time. With a lymphocyte count of about 260,000, hemoglobin of 9.4, and platelets finally having dropped to a Stage 4-level 85, the need for treatment is staring me squarely in the face, if not also socking me squarely in the jaw.
I have spun the wheel of fortune and picked a name from the measly list my health plan offers. I'll be seeing the new name soon, and hopefully I'll like this person enough to make them my new onc. Meanwhile, I won't rule out seeing Dr. Tower. But since insurance won't cover treatment at that practice, it may be time to cut the cord and go. Especially since it has been pretty much cut for me.
Ouch.
And on January 27, Dr. Tower wrote to Dr. Belle's patients:
"Dr. Belle has recently informed us, and sent a letter to you, stating that she will be leaving the practice effective 1/30/12. Let me assure you that our office still remains committed to serving your needs and assisting in your care. I understand that Dr. Belle's departure may be upsetting to you, but I assure you that I am more than willing and able to assume your care, and would in fact be honored to do so . . ."
There is no doubt an interesting back-story here, which I don't imagine I will ever know. For me and for Dr. Belle's other patients, the big news is that we don't have a doctor anymore. Dr. Tower wants us to stay, but I hear through the grapevine that a number are choosing to go.
For me, all this comes at the worst possible time. With a lymphocyte count of about 260,000, hemoglobin of 9.4, and platelets finally having dropped to a Stage 4-level 85, the need for treatment is staring me squarely in the face, if not also socking me squarely in the jaw.
I have spun the wheel of fortune and picked a name from the measly list my health plan offers. I'll be seeing the new name soon, and hopefully I'll like this person enough to make them my new onc. Meanwhile, I won't rule out seeing Dr. Tower. But since insurance won't cover treatment at that practice, it may be time to cut the cord and go. Especially since it has been pretty much cut for me.
Ouch.
Let's say you're a patient with a low income who qualifies for help from a drug company. That drug company is willing to deliver the drug, free of charge, to an infusion center near you.
Great, right?
And let's say your insurance is contracted with Scottsdale Chemo Hut. (Sure, it would be nice to get the infusion done at your oncologist's office, but your insurance won't cover treatment there, even though it will cover office visits. That is the sixth circle of Hell, which has more circles than Saturn has rings when it comes to health insurance issues.)
So let's say you are getting everything set up with Chemo Hut, and in the process you speak to the pharmacy manager. And you are told this: Chemo Hut does not accept drugs directly from drug companies. The drug can arrive in an armored vehicle, in a suitcase chained to the wrist of the president of the company, and they'll still refuse to accept it.
And why is this? Because Chemo Hut cannot bill for it. If they use their own supplier, they can make money. Increasingly, more hospitals and infusion centers are refusing to administer free drugs that their patients qualify for. This is because they are upset about a trend known as "white bagging."
Under white bagging, insurance plans use their own specialty pharmacies to supply drugs at a cheaper rate than those purchased through the hospital supply chain. By some estimates, this now accounts for some 25% of infusions. Complimentary drugs for the less financially fortunate are collateral damage in this tug of war between insurers, who want to contain costs, and hospitals, which want to maximize profits.
Hospitals also complain about the inconvenience of having to store these drugs separately and write things like "for David Arenson only" on the outside of the box.
FYI, there is also something called "brown bagging," in which the drug is delivered to the patient, who totes it in along with their lunch. Maybe I can see that one being a problem. Chemo Hut may not want to be responsible for infusing you with ofatumumab you bought off a guy in a truck down the block.
Still, for patients who need chemotherapy and who cannot otherwise afford it, Chemo Hut and other hospitals and centers are making no exceptions, and this makes life difficult, not to mention a little more absurd than it already is.
In my case, Chemo Hut will infuse the drug if it is ordered through their supplier; our insurance company does not work with specialty pharmacies, and it has approved the drug under my medical benefit, which means I have to pay 20% coinsurance. Or, we estimate, upwards of $20,000 by the time all is said and done.
Well, lucky me, Chemo Hut also has a financial assistance program. A patient may qualify for a reduction in the bill of up to 100%. I say "may" and I use the term guardedly, because a patient may also not qualify, and be stuck with angry collection agencies and dings on their credit if they are unable to pay. The coinsurance the patient owes must now be written off as a loss. And while the insurance company will pay 80% at a negotiated rate, there is probably not a huge amount of profit there. So how much money is Chemo Hut actually making when all is said and done?
Chemo Hut could have administered free drug and still earned money on the costs of infusion, which is not chump change. But that would have been too easy. I know from running a business that sometimes you sell something and make a lot of money, and sometimes you sell something and make a little, but that you need both kinds of sales to stay profitable. (Not to mention the moral issues involved, but we're talking the health care system here, so that may not apply.)
There is one alternative, perhaps. One might ask the insurance company to approve infusion of the drug in the oncologist's office after all. The oncologist doesn't have a problem with white bagging because the oncologist actually cares about the patient. The oncologist, BTW, would like to be "in network" with the insurance and is willing to negotiate a fair price.
All of this would save the insurance company from having to pay huge sums of money for an expensive drug that can be gotten for free. Compared to the costs of the drug, paying the cost of administration is a substantial savings.
The savings would be, as they say on Vulcan, logical. This is Earth, though, specifically the United States. The insurance company (and Chemo Hut) would rather create a ridiculous financial morass that benefits no one, including the patient.
Just a little update. Marilyn (She Who Battles Insurance) and I are working on getting our ducks in a row. I have an appointment in early February with a doctor who is managing some clinical trials of Btk inhibitors. And in the meantime we are working on getting O+HDMP set up as a fallback.
"O" stands for "ofatumumab," aka Arzerra. Apparently it is a strange and unusual beast. We're working with one of the largest hospitals (where the infusion would take place) in one of the largest metropolitan areas (Phoenix) in the country, and ain't nobody never asked for none of that fancy 'tumumab stuff before. The inventory control manager of the hospital pharmacy is trying to figure out what it is and how to get hold of it.
 Of course, all of this
would be much easier if I could just have the infusion at my
oncologist's office. But she's out of network, even though insurance
will pay for me to see her. They just won't pay her to treat me. And
this is why my brain is turning to mush, which is an unexpected side effect not of CLL, but of having American health insurance.
Surprisingly, it appears that insurance will approve ofatumumab -- under my medical benefit, not my pharmacy benefit. Medical benefit means it has to be "injected at the hospital," and I will owe 20% coinsurance. Pharmacy benefit means it's a drug with a $35 co-pay. Near as we can tell, I am going to be on the hook for something like $17,000 in coinsurance if I can't get some help from somewhere. Which means I can't afford it, unless I'd like to consider going bankrupt.
I am reminded of the late Dr. Terry Hamblin's many posts in which he discussed the merits of one drug or another, compared often negligible differences in progression-free survival, and concluded that the beaucoup expensive drug was not worth the cost. O+HDMP could turn into R+HDMP, I suppose, or chlorambucil plus prednisone, which costs almost nothing.
Meanwhile, maybe a trial will work out. . . . The big question is how a Btk inhibitor might affect marrow function. My hemoglobin is down to 9.6, and slowly trending south. Welcome to Stage 3.
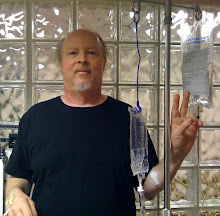
What I do know is that some kind of treatment has to come soon, and February looks like the month. I'll report back when I'm finally sitting in the chair somewhere, having something happen.
Of course, all of this
would be much easier if I could just have the infusion at my
oncologist's office. But she's out of network, even though insurance
will pay for me to see her. They just won't pay her to treat me. And
this is why my brain is turning to mush, which is an unexpected side effect not of CLL, but of having American health insurance.
Surprisingly, it appears that insurance will approve ofatumumab -- under my medical benefit, not my pharmacy benefit. Medical benefit means it has to be "injected at the hospital," and I will owe 20% coinsurance. Pharmacy benefit means it's a drug with a $35 co-pay. Near as we can tell, I am going to be on the hook for something like $17,000 in coinsurance if I can't get some help from somewhere. Which means I can't afford it, unless I'd like to consider going bankrupt.
I am reminded of the late Dr. Terry Hamblin's many posts in which he discussed the merits of one drug or another, compared often negligible differences in progression-free survival, and concluded that the beaucoup expensive drug was not worth the cost. O+HDMP could turn into R+HDMP, I suppose, or chlorambucil plus prednisone, which costs almost nothing.
Meanwhile, maybe a trial will work out. . . . The big question is how a Btk inhibitor might affect marrow function. My hemoglobin is down to 9.6, and slowly trending south. Welcome to Stage 3.
What I do know is that some kind of treatment has to come soon, and February looks like the month. I'll report back when I'm finally sitting in the chair somewhere, having something happen.
The CLL community has lost one of its best and truest friends, Dr. Terry Hamblin, to his own battle with a different cancer.
Hamblin, one of the world's leading chronic lymphocytic leukemia doctors and researchers, retired from most of his duties in the U.K. about six years ago. He could have gone sailing, or found a lucrative post with a pharmaceutical company, or disappeared into a quiet, well-earned country life. Instead, he rolled up his sleeves and went to work where he was needed most, using new internet tools to help CLL patients worldwide.
I began my blog in November 2005 and Terry's came on line just a couple of weeks later. Through his blog and his inexhaustible contributions to the ACOR CLL List, not to mention personal e-mail, Terry answered thousands of questions about the disease and its treatment. He freely gave of his lifetime of experience, even to the point of exhaustion. Over at ACOR they established something called The Professors' Posts to archive his answers so the same question did not have to be asked of him again and again (the plural in professors includes another invaluable ACOR contributor, Dr. Susan LeClair).

I called him Terry, but I always felt a little awkward about it. It's sort of like calling God "dude." He signed everything "Terry Hamblin," in the matter-of-fact way that was his trademark. When he got rushed, he tended to transpose the letters in "the," and there was always a place in my mind where I saw him as "Teh Professor." And I mean that respectfully and lovingly. In a world where our written words -- in e-mails, blog posts, discussion forums -- have become our main form of communication with one another, there are little tics, little traits that you notice.
Another thing I noticed was that Terry was always honest and direct. He told you what he thought, and he told you if he didn't know something, and he never made an effort to sugar-coat anything. In other words, he treated us patient rabble like people, like equals, like adults.
"We [doctors] really don't have the means to keep you alive for longer than about 12 years," he once wrote to me. It wasn't what I wanted to hear, but it was the truth as he saw it. That's one thing you could count on hearing from Terry Hamblin.
Terry was a bit old school. He believed in the scientific method. He had seen too many things come and go to jump on the latest bandwagon. He wasn't the cheerleader type. He liked hard evidence, and so he provided a grounded, conservative perspective as new treatments and tests unfolded. This didn't always make him the most popular voice out there, but you could always rely on him for sure and steady reasoning.
I never detected an atom of pomposity in the man, and this is no small feat in a world in which "M.D." is sometimes taken to mean "Medical Deity." Terry didn't need to have his ego stroked, and while he was justly proud of his many accomplishments, he remained, as far as I could tell, a humble, uncomplicated soul. It was as if he didn't see the invisible line that we patients see between doctors and ourselves. To him, we were all just people, and when he began his struggle with his own cancer, we CLLers came to see the full scope of his strength, his vulnerability, and his humanity. Terry was now on the journey that we had been on, experiencing the travails of cancer that go beyond medicine.
Over the years, I tried not to bother Terry too much, knowing how many inquiries he received, but I did correspond with him from time to time. He once went out of his way to discuss my case with some of the best minds in U.K. hematology, a favor I did not expect nor ask for, but for which I was grateful. He read my blog sometimes and occasionally commented here, which made me feel like maybe I wasn't a complete idiot.
Readers of his blog know that Terry Hamblin was a devout Christian. But he not only talked the talk, he walked the walk.
Last November, Terry wrote something that sums up his character in far better words than any I can offer:
I had a weepy day yesterday as I contemplated the things I had left
undone. At the end of Schindler's List, Liam Neeson has a scene
where he looks at his luxury car and his gold ring and thinks of how
many more Jews these could have bought. "I could have done more," he
exclaims.
That is how I felt. I told this to Dr John when he
visited and he reassured me. None of us can ever do enough. We mustn't
reproach ourselves.
Today I am much more cheerful. I went out for
the first time in 2 weeks and bought some flowers for my wife. The
Scripture tells us not to be weary in well-doing.
Terry never truly tired of well-doing, and he left
a world of good works in his wake. There is no better testament to a
life well-lived. He will be sorely missed in this little corner of Arizona, and by his friends everywhere across the globe.
It's 2012, and my CLL journey continues along a new stretch of Shit Creek. I am, at the moment, paddle-free.
But let me take a moment to wish you all a Happy New Year. May we continue on in enough good health to continue on, and may we have time left over after dealing with medical matters to enjoy our lives, our loved ones, and the beauty and bounty that the Earth provides.
It's important to keep that perspective, even in difficult times. As you know, I lost my older brother to a stroke six months ago, so mortality seems that much more fragile to me than it did before.
Then, this morning, I scrolled through the list of blogs I keep on the right side of this page and found that another CLL compatriot, Jackie Sue, has passed on.
Everywhere in CLL World I see struggle; often with enough success to keep on fighting another day, sometimes with less success than was hoped. And all this is occurring against a rather jaw-dropping array of new progress in CLL, namely the kinase inhibitors such as CAL-101 and PCI-32765 and the CAR trials of juiced up killer T-cells, such as CART-19 at the University of Pennsylvania. (This PDF from CLL Global gives a good, brief rundown on both.)
I cannot help but conclude, as I think of friends I have lost, as I think of those who are struggling as I am, how close we are to salvation, and yet so far.
I blog less these days. One big reason is that I am busy with our ever-growing and ever-demanding online business, not to mention personal matters, usually my health and that of my dear Marilyn.
But when there is a little time left over, I find myself hesitating to write. In part, I have run out of useful things to jabber about. My training as a newspaper editor etched into my head that a story has to be worth being told to merit space in print.
Another reason is, for lack of a better term, battle fatigue. You can paint lipstick on the CLL experience, but it's still a pig, and after eight years I have seen enough pain, suffering, and life-altering disruption to conclude that having CLL completely and totally sucks. There's nothing good to be said about it, and therefore I find myself not wanting to talk about it.
That said, it was my promise when I started this blog to describe my journey honestly and completely, so that my experience will be a useful learning tool for those who come along. And so, the latest:
The good news is that the abscess referred to in my last post has healed, the drain has come out of my neck, and the infection is gone. The node in question has not enlarged very much; indeed that side of my neck shows less nodeyness than the other. Perhaps if we CLLers stick drains in our nodes the disease will simply drip away. (Yes, I'm kidding.)
The bad news is that my disease has entered a new, more aggressive phase. For the first time, my red counts have dropped due to marrow impaction. My hemoglobin has been in the 10 to 11 range for the past couple of months. Platelets have also fallen, to just above 100. I am on the doorstep of Stage 4, measuring by those numbers.
What's worse, the nodes have returned with a vengeance, that one area of my neck aside. My guess is that this is simply the product of ineffective control of the disease for many months, as opposed to some new mutation. Until I have a FISH test, I won't know for sure.
Let's back up for a minute. I'll try to cover some history, briefly, that would have made for several blog posts had I had the time.
After a year of treatment, I went off Revlimid (lenalidomide) last March, in part because I wanted to give my body a break. As you may recall, I had two transient ischemic attacks while on the drug. Clotting problems run in my family and claimed the lives of both my brother and my mother.
Another reason was the expectation that I might qualify for a CAL-101 clinical trial. I will call this the Godot trial, because I kept waiting and waiting and waiting for a slot to open, and was told "any day now" for what became months and months. What was supposed to have occurred in April was delayed until August. Even then, it all seemed rather promising. I had restarted Revlimid in July because the need to treat could wait no longer. Calistoga, the maker of CAL-101, was even willing to waive the requirement that I should not have had treatment 28 days before enrolling. When I was about to pack my bags, I got the bad news: due to a clerical error, the slot in question did not exist. And they could not just add a new one, since the maker of the other drug in the trial, ofatumumab (aka Arzerra), would not provide any more free drug.
I was told that drug companies hire other companies to organize and manage trials for them, and that one of these companies had made the mistake. The principal investigator was quite aplogetic and said this had never happened in all the years he had been conducting trials. Goodbye, paddle.
Meanwhile, back at Revlimid Ranch, things weren't going so well. When I restarted the drug, I did so with a great deal of care paid to the clotting issue. At the time I began Revlimid 2.0, my brother lay in the hospital, unable to move his left side and barely able to move his right.
I had a
complete clotting panel done, which confirmed my propensity to clot. Indeed, it came out worse than a similar panel that was run on my brother.
I had been on warfarin for a little while prior to quitting Revlimid in March, but my clotting time always remained pretty much normal, which means fast. And so when I began Revlimid again, we
added more warfarin, to which, it turns out, I don't easily respond. Later, my doctor added aspirin to the warfarin. Meanwhile, the Revlimid dose was kept
minimal, at 5 mg twice a week and occasionally every other day. As it turns out, I wasn't getting enough of the drug.
In November came the first signs of trouble. My red counts showed a drop, and my lymphocyte count showed a jump. Shortly thereafter, I began to notice an orange cast to my urine. I've posted about that several times, and in the past it had always been a sign of hemolysis due to autoimmune hemolytic anemia (AIHA). I assumed that was the case this time as well.
Revlimid, an immunomodulator, had seemed to put an end to my AIHA. Tests were ordered, and in the meantime I went on Revlimid 5 mg daily in an effort to head the hemolysis off at the pass. It made sense at the time: Maybe I needed more Revlimid to control the situation.
But the testing showed no signs of AIHA, and also that red counts were continuing to drop. And the orange urine remained, which brought me to the next logical conclusion: internal bleeding due to blood thinners.
So I stopped the thinners and the orange disappeared almost immediately. And no blood thinners meant no Revlimid, which was coincidentally giving me new fits in terms of tumor flare. (Goodbye, other paddle.) After merely five days of 5 mg, the minimal dose Celgene makes and well below that considered optimal in trials, I looked freakishly flarish (see second-to-last photo in my last post).
I had always had a tumor flare reaction with Revlimid, which is actually a sign that the drug is working, but never anything like this.
It felt like a Vise-Grip was closing around my neck from the back, leaving just a bit of my Adam's Apple free, and making it hard to open my mouth very far. It was at this point that the abscess formed, although it took another week, during which steroids brought down all the flare but the abscess, before I ended up in the ER and the diagnosis was made.
During the December Drain Festival, I could not treat the CLL because of the wounded node. Now that it has been removed, and the node is healing -- the ENT doc says to give it at least two weeks -- treatment is back on the table.
I am looking into a couple of clinical trials, as well as into a treatment to keep me going in the interim. One thing I have learned about trials, of course, is that Things Take Time. Another thing I have learned is that the study drug may be free, but all other expenses, from administering the drugs to CT-scans to the cost of the drug that the study drug is being tested with, are usually out-of-pocket. Unless covered by insurance (insert guffaw here).
The treatment I may do soon is R+HDMP, or perhaps Arzerra plus HDMP, which is a whole 'nother can of worms.
I've been stymied at every turn by my increasingly stingy health insurance plan, which covers fewer and fewer doctors -- including treatment in the office of my own oncologist -- and fewer and fewer drugs. Clinical trial expenses, forget it. And while Arzerra may have FDA approval for CLL, to borrow a phrase from a popular viral video, honey badger don't care.
It's gotten so bad that I've found myself flirting with the idea of dropping coverage for six months so that I can get on the new federal Pre-Existing Condition Insurance Plan. I know, this is probably a bad idea, especially since my little hospital getaway (two fun-filled nights and three fun-filled days) came to more than $10,000, of which I will end up paying no more than a third thanks to my insurance, bad as it is
(I am so looking forward to 2014, when I'll be able to buy decent insurance under the new health care law. I have my issues with President Obama, but from where I sit, he deserves a big, wet kiss for Obamacare, imperfect as it is.)
The cherry on the sundae is that there is a fair degree of tumult at my oncologist's office that is also not helping matters.
So let's just say that external forces are not making my little canoe trip an easy one. Shit Creek is hard enough to navigate with a paddle.
But onward I go, mateys, trying not to capsize.
To quote Newt Gingrich (yes, I am quoting Newt Gingrich):
Perseverance is the hard work you do after you get tired of doing the hard work you already did.
 And on January 27, Dr. Tower wrote to Dr. Belle's patients:
And on January 27, Dr. Tower wrote to Dr. Belle's patients: