There are three things I know about my health, and all else is pure conjecture:
I have cancer.
I am going to die.
I may not die of cancer.
A lot of people do not make the final connection. I recall a post on the internet by an otherwise erudite CLL patient who said, “Well, at least we know what we’re going to die of.”
That, my friends, is stinkin’ thinkin’, as Al Franken’s “Stuart Smalley” character used to say. There is plenty of evidence that CLL is not inevitably fatal. And as treatments improve, so will the odds. Various reports say that somewhere between one third and one half of us will survive it an
 d go on to die of the usual stuff: flying anvils, using portable toilets at county fairs, and breath-sucking cats. (And remember that those CLL survival reports are based on older data, from an era of less effective treatments that were applied without today’s improved prognostics and risk-based thinking.)
d go on to die of the usual stuff: flying anvils, using portable toilets at county fairs, and breath-sucking cats. (And remember that those CLL survival reports are based on older data, from an era of less effective treatments that were applied without today’s improved prognostics and risk-based thinking.)Yet society still tends to think most cancer patients are doomed. This attitude permeates into the medical establishment as well and perhaps accounts for the rather callous way in which some patients can find themselves treated. Many CLL patients subconsciously accept this misjudgment as a verdict on their condition, and therefore they develop a certain tunnel vision when it comes to treatment: If it helps me today -- no matter what the side effects may mean for my future treatment prospects -- then that’s good, because I probably won’t live that much longer anyway. After all, I have an incurable cancer. Why worry about ten or twenty years from now?
Why worry? Because expectations, and the decisions that flow from them, can make all the difference to your survival. Lower your expectations, and you can expect less in terms of results.
In his book Love, Medicine, and Miracles, Dr. Bernie Siegel describes the three types of cancer patients he has encountered: The first group, around 10 to 15 percent, actually want to die. Their diagnosis comes as some sort of relief, and it usually becomes a self-fulfilling prophecy.

The second group, around 70 percent, would like to live but don’t really want to be bothered with doing everything possible to figure out how. They’ll dutifully do what the doctor says, but they won’t ask many questions, and they won’t go looking on their own for information about their disease and how to treat it. They also won’t make changes, such as learning to cope with stress or giving up bad habits, that could increase their chances of living a longer life. This might be described as the couch potato method of dealing with a medical crisis.
The third group of 10 to 15 percent are what Siegel calls “exceptional” cancer patients. These are the people who raise their hands when he asks, “Do you want to live to be 100?” They have high expectations for themselves, and they have high standards for their medical caregivers to meet. They have a take-charge attitude, want to know everything about their disease, and aren’t afraid to confront doctors, nurses, health insurance companies, etc. when necessary. They also try to come to grips, emotionally and spiritually, with their situation, to find new energies and coping skills that can turn a lemon into lemonade. And here’s their reward: According to Siegel, studies show that these sorts actually do better in the fight against cancer. Treatments work better, and they live longer.
In a recent article in The New York Times, the son of the late author Susan Sontag described her battle with breast cancer in the 1970s:
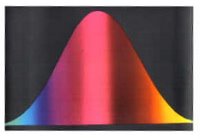
During the two years of chemotherapy she underwent in the mid-1970's to treat her first cancer - Stage 4 breast cancer that had spread into 31 of her lymph nodes - she managed to publish a book on photography and, a year later, her book "Illness as Metaphor." That time, she had beaten the odds. William Cahan, then her principal doctor at Memorial Sloan-Kettering Cancer Center in New York, told me at the time that he saw virtually no hope. (Those were the days when doctors often told patients' relatives things they did not disclose to the patients themselves.) But as her friend Dr. Jerome Groopman, chief of experimental medicine at the Beth Israel Deaconess Medical Center in Boston, told me a few months after her death: "The statistics only get you so far. There are always people at the tail of the curve. They survive, miraculously, like your mother with breast cancer. Her prognosis was horrific. She said: 'No, I'm too young and stubborn. I want to go for it"' - meaning treatment. "Statistically, she should have died. But she didn't. She was at the tail of that curve."
So how do you get to the tail of the curve? Raising your expectations is a good way to start. If our struggle
 with CLL is a long, drawn-out fight, then let us remember that morale is a factor in war. It is those who expect to win that often do, and not because their expectations magically make them invincible. It is because they have qualities that give legitimate rise to their optimism: bravery, tenacity, patience, the skill to acquire good intelligence about the enemy, and an ability to come up with the best strategy and tactics. Of course, adequate weaponry helps. And luck, too, is part of the picture.
with CLL is a long, drawn-out fight, then let us remember that morale is a factor in war. It is those who expect to win that often do, and not because their expectations magically make them invincible. It is because they have qualities that give legitimate rise to their optimism: bravery, tenacity, patience, the skill to acquire good intelligence about the enemy, and an ability to come up with the best strategy and tactics. Of course, adequate weaponry helps. And luck, too, is part of the picture. My guess is that someone reading this post –- or maybe two people, or three, or four, and perhaps even more -– will confound all those with lowered expectations and be at the tail of the curve.
It could be you.





3 comments:
Dear David,
You must be talking about me, the end of the curve. And good old dumb luck or is that the same thing?
I am 15 months out from a SCT and doing just fine. I have not had as much as a cold let alone all the terrible things that befall our friends on the List. There were some rough days around the time of the transplant, to be sure, but I had the benefit of each day being better than the one before, no set backs, so far.
I wonder why there are not more transplants. Maybe it is my age (now 53) relative good heath, matched siblings, or the urging of my doctors, great heath insurance. All those were and are working for me, for sure.
Thank you for all of your fine writing, I enjoy your blog. Matt
I plan on beating the curve. Thanks again for your blog. Elyse
Post a Comment