But what is hope, exactly? And how does it affect the course of disease?
Some answers can be found in a well-written and thoughtful book called The Anatomy of Hope: How Pe
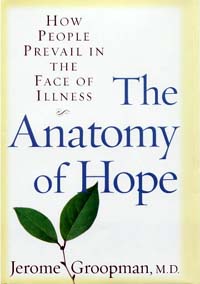 ople Prevail in the Face of Illness, by Dr. Jerome Groopman. Groopman is a hematologist/oncologist and the chief of experimental medicine at the Beth Israel Deaconess Medical Center in Boston. He has practiced medicine for several decades and for nearly 20 years was a patient himself, suffering from a chronic back condition. Level-headed and science-minded, Groopman provides some insights into what hope is, and what it is not. His search is for the middle ground, “where both truth and hope reside.”
ople Prevail in the Face of Illness, by Dr. Jerome Groopman. Groopman is a hematologist/oncologist and the chief of experimental medicine at the Beth Israel Deaconess Medical Center in Boston. He has practiced medicine for several decades and for nearly 20 years was a patient himself, suffering from a chronic back condition. Level-headed and science-minded, Groopman provides some insights into what hope is, and what it is not. His search is for the middle ground, “where both truth and hope reside.”Groopman began his medical career in the 1970s, when doctors were trained to deal with the clinical aspects of disease, not the human ones. There was a tendency to view people as collections of symptoms and test results, passive participants in the medical process. Over time, Groopman realized the limits of his training. He encountered some remarkable patients who taught him a great deal about how human emotions and expectations could affect the clinical outcome of disease, both positively and negatively.
When it came to balancing truth and hope, Groopman as a young doctor went overboard one way, then the other. At first, he avoided telling patients much about their conditions, believing this would foster a sense of hope. When patients became angry and resentful that he had not been honest, Groopman took the opposite tack: telling them the cold, hard facts. This included the now-outdated “you have two years to live” sort of thing, which Groopman abandoned after one patient lived to just the expected two years, after which her family informed him that she had been miserable the whole time, waiting for the clock to run out.
(To be fair, patients do not always agree about what they want to know. In CLL, some patients roll their eyes when they are told they have “the good cancer,” but there are no doubt others who are thrilled to hear it. For some patients, knowledge is power; for others, ignorance is bliss. It is the doctor’s delicate role to finesse each patient’s level of interest and involvement while still insuring that the individual gets a basic overview of the medical facts. This is why the cues you send your doctor -- verbally, emotionally, even in terms of body language -- are so important.)
Eventually, Groopman was to conclude that “omniscience about life and death is not within a physician’s purview. A doctor should never write off a person a priori. At the moment of initial diagnosis, closing off options and denying choices is premature and clinically wrong.”
Exceptions to the rule
Groopman reached that conclusion because he discovered that there are some people’s diseases that “did not seem to read the textbook.” He talked of one patient who “didn’t surrender from the start, and not surrendering has sustained her life.” Another, a fellow physician named George, beat stomach cancer, where the odds were 99% in favor of fatality, through sheer will and excruciating chemotherapy and surgery.
“The mustering of the will to engage the foe and the strength to sustain the battle, in themselves, became a form of victory,” Groopman writes. Later, he adds: “To hope under the most extreme circumstances is an act of defiance that, as George explained, permits a person to live his life on his own terms. It is part of the human spirit to endure and give a miracle a chance to happen.”
These miracles, Groopman takes pain to emphasize, are medical ones, a
 nd they are rare. Sometimes hope cannot put off the inevitable, but it can make the road to the end easier. As such, hope can take many forms.
nd they are rare. Sometimes hope cannot put off the inevitable, but it can make the road to the end easier. As such, hope can take many forms.One patient, Barbara, fought her cancer with equanimity and good humor. Groopman detected none of the seesaw of emotions that we associate with such a battle.
“Barbara Wilson’s unique calm and acceptance were present from the outset -- not surrender, but steady realism; she set the parameters on her care with a clear-eyed vision of what was possible, what made sense to her, how she wanted to live, when it was time to die. . . . Barbara did not cling to a desperate belief that I would arrive at the bedside with a cure from the laboratory just in the nick of time, though I deeply wish such a moment had occurred . . .
“Barbara’s hope was real and undying . . . it reflected the fact that she had found purpose and created meaning in her life through relationships with her loved ones, and with her God. Barbara did not dwell on the ineffable questions “Why me?” and “Why now?” She saw death as a natural part of life. It is not necessary to be a person of profound faith to hold this view and to act on it. I sensed that my father had the same approach to life and death. Personal philosophy and experience, rather than faith, seemingly prepared him to acknowledge the reality of his mortality.”
Hope, then, can be seen both in will, and in acceptance. This may seem contradictory, but it isn’t. Hope is what gets us through the experience of our disease. Depending upon our personalities and our medical conditions, it may take different forms.
Searching for the mind-body connection
The mind-body connection comes under scrutiny in the book as Groopman searches for a “biology of hope,” science-based evidence to support the improvements and cures that he has seen defy the odds.
Through Groopman’s interviews with some leading researchers in this nascent field, we learn that some aspects of this biology are coming into focus, though we are far from understanding exactly how it works.
Dr. Bruce Cohen, a professor at Harvard Medical School, talked about mind, body, and soul. Our emotions, thoughts, perceptions, and desires appear to be a product of “mind,” and therefore somehow disembodied, “hovering in an ether several inches above our heads.”
“Of cou
 rse,” Groopman quotes Cohen as saying, “this is not the case. ‘Mind’ is a manifestation of brain. What we view as products of the mind -- thoughts, feelings, and emotions -- are a mighty mix of chemicals and electrical circuits that have evolved over the millennia, and still are changing. So, too, is consciousness -- our memory of the past, awareness of the present, and anticipation of the future. ‘Body’ includes brain, and thus mind, so that the construct ‘body-mind connection’ only emphasizes the artificiality of how we have traditionally divided them.”
rse,” Groopman quotes Cohen as saying, “this is not the case. ‘Mind’ is a manifestation of brain. What we view as products of the mind -- thoughts, feelings, and emotions -- are a mighty mix of chemicals and electrical circuits that have evolved over the millennia, and still are changing. So, too, is consciousness -- our memory of the past, awareness of the present, and anticipation of the future. ‘Body’ includes brain, and thus mind, so that the construct ‘body-mind connection’ only emphasizes the artificiality of how we have traditionally divided them.”(“Soul,” Cohen added, is something else again, “a fundamentally metaphysical and religious concept where the divine spark resides.” The soul is not the product of “cerebral chemicals and neuronal circuits.” There is no way for scientists to “experimentally locate or characterize such a metaphysical entity. It was beyond science; it was a matter of faith.”)
Cohen recommended that Groopman study the placebo effect, and Groopman details accounts where it has been found to be real. The placebo effect can change the autonomic nervous system, help control asthma, speed recovery from a heart attack, reduce joint pain, and help release dopamine from “untapped” areas of the brain, which is an aid to those with Parkinson’s Disease. Hope can, in actual practice, release chemicals in the brain that make one feel better.
“Within our brains are chemicals akin to opiates,” Groopman writes. “These chemicals are called ‘endorphins’ and ‘enkephalins.’ Belief and expectation, cardinal components of hope, can block pain by releasing the brain’s endorphins and enkephalins, thereby mimicking the effect of morphine.”
There is a flip side. Groopman points out that physical pain and deterioration can feed our anxieties and confirm our worst fears. This has the effect of reducing the outflow of the brain’s “good” chemicals, and perhaps heightening those, such as cholecystokinin, or CCK, which can amplify the pain circuitry.
“This is a vicious cycle,” Groopman writes. “When we feel pain from our physical debility, that pain emphasizes our sense of hopelessness; the less hopeful we feel, the fewer endorphins and enkephalins and the more CCK we release. The more pain we experience due to these neurochemicals, the less able we are to feel hope.”
Sometimes treatment of physical symptoms can help restore a patient’s sense of hope and well-being, presumably with a resulting chemical cascade in the brain.
Take fatigue, for example. This is a common complaint among CLLers, and Groopman uses as an example the case of a depressed CLL patient. Her anemia was gradually worsening, and so was her sense of despair, Upping her dose of erythropoietin, to boost red blood cell production, changed her attitude.
The patient told Groopman she felt better. “I’m still tired,” she said. “But not like I was, so fatigued that I didn’t want to move out of bed in the morning.” Groopman writes: “It was as if the relentless signals from her tissues, demanding hemoglobin and the gift of oxygen, had crowded every corner of her mind and allowed no room for hope.”
Hope deconstructed
It is in his interview with Wisconsin Professor Richard Davidson, an experimental psychologist and expert on positive emotions, that Groopman “deconstructs” hope, getting at its essence.
Hope, Davidson posits, is “an emotion made up of two parts: a cognitive part and an affective part. When we hope for something, we employ to some degree our cognition, marshaling information and data relevant to a future desired event.” A cancer patient, for example, has to generate a different vision of his or her condition. “That picture is painted,” Davidson explains, “in part by assimilating information about the disease and its potential treatments.”
But hope also involves a second component, what Davidson calls “affective forecasting – that is, the comforting, energizing, elevating feeling that you experience when you project in your mind a positive future.”
Together, these components “interweave and modify each other.”
Dr. Antonio Damasio, a professor of neurology at the University of Iowa, argues that emotions are “cognitive guides, fostering the process of logic rather than retarding it.”
Hope and other emotions, Groopman writes, can “powerfully influence cognition and other deliberative feeling. They impact the machinery of perception, the circuits that are used to take in and process data and make decisions.”
In other words, as one of my CLL heroes -- the late David Covell -- once put it, hope is an active process. And an essential one for any cancer patient to get a handle on.
Even before reading Groopman’s book, I had the intuitive sense that hope was more than just an emotion. After reading the book, I think it can be seen as the synthesis of emotion and rational thought into a realistic plan for a better future. Creating this vision allows the patient to be proactive and intelligently involved in medical care. Hope is, perhaps, the difference between wanting to do something, and having to.
As time goes on, new information and circumstances can cause us to adjust the vision that arises from our hope, but as a rule hope stands the test of tough times. Once firmly established, it is hard to uproot.
True and false hope
In his final chapters, Groopman looks at hope as a tool for coping with disease.
“While it is a convenient construct to divide hope into a cognitive and an affective component, the two are tightly coupled. Feelings and emotions mold logical feelings and deliberate decision making . . . True hope, then, is not initiated and sustained by completely erasing the emotions, like fear and anxiety, that are often its greatest obstacles. An equilibrium needs to be established, integrating the genuine threats and dangers that exist into the pr
 oposed strategies to subsume them. So when a person tells me that he doesn’t want to know about the problems and risks, that he believes ignorance is necessary for bliss, I acknowledge that yes, unbridled fear can shatter a fragile sense of hope. But I assert that he still needs to know a minimum amount of information about his diagnosis and the course of his problem; otherwise, his hope is false, and false hope is an insubstantial foundation upon which to stand and weather the vicissitudes of difficult circumstances. It is only true hope that carries its companions, courage and resilience, through. False hope causes them to ultimately fall by the wayside as reality intervenes and overpowers illusion.”
oposed strategies to subsume them. So when a person tells me that he doesn’t want to know about the problems and risks, that he believes ignorance is necessary for bliss, I acknowledge that yes, unbridled fear can shatter a fragile sense of hope. But I assert that he still needs to know a minimum amount of information about his diagnosis and the course of his problem; otherwise, his hope is false, and false hope is an insubstantial foundation upon which to stand and weather the vicissitudes of difficult circumstances. It is only true hope that carries its companions, courage and resilience, through. False hope causes them to ultimately fall by the wayside as reality intervenes and overpowers illusion.”I would argue that, in CLL, the bar of “knowing a minimum amount of information” about our diagnosis and its course is far higher than in most cancers. This is simply because, as has been well-established, the disease is idiosyncratic, treatments are all over the map if one treats at all, and even the experts disagree on what to do. Therefore, the cognitive element of hope -- the process of marshaling information and data -- is more complex, but no less essential.
What is clear from The Anatomy of Hope is that we patients cannot sit back and expect hope to happen to us. It is an active process, something we must create, and recreate when necessary. Part of this is learning, part of it is intuiting, all of it is essential if we want to live longer.
Hope is a mechanism that optimizes our ability to function. Groopman calls hope “as vital to our lives as the very oxygen we breathe.” As a doctor he searches for it whenever he sees a new patient.
We patients, too, must search within ourselves for it.
As Groopman concludes:
“Patients are awash in a sea of statements about their emotions and their maladies. For years I diverted or dismissed their inquiries because I did not know how to answer. Now my response is formed by the lessons taught to me by my patients and the stirrings of serious science. I recount some of the narratives here, and say we are just beginning to appreciate hope’s reach and have not defined its limits. I see hope as the very heart of healing. For those who have hope, it may help some to live longer, and it will help all to live better.”






5 comments:
David-
A great review of the book. I plan to buy it this weekend and give it to Tom. He is full of hope and it is easy to see but when he has an infection, I notice that his "hope barometer" goes down. Makes sense.
Welcome Home! I'm so glad to see that you are back. I have heard of Dr Groopman and his book but haven't yet read it. I will now. I have mostly had a positive outlook in my life and never questioned my hope. I've more questioned those who exist without it. As I was going to sleep last night, after having read your report, I imagined life without hope and realized what I would NOT be doing if I didn't have it...planning a retirement in a few years with my husband, imagining our childrens' weddings in the future, accepting freelance assignments that go for 3 or more years. There's a difference between the everyday belief that none of us knows how long we are here - healthy-ill-chronic or otherwise - and living with more knowledge than some have and still keeping hope alive. I am one of those who doesn't believe CLL is necessarily a good cancer but it certainly is better than many. The hardest thing for me at first was the W&W...I wanted to do something. Now, I've accepted W&W. When I hear some say "why me?" I often wonder "why not?" Enough already - thank you for your blog - let us know what's next for you.
Nice review. I have not (yet) read the book, but it sounds as if it agrees with some research we have been doing at our place.
We had been having problems with nurses and other caregivers pressuring us to give up on certain patients when we felt the patients still had a glimmer of hope, and the patients were willing to perservere.
We set up a study and found that patients with cancer want a chance to live -- even in the face of dim odds. On the other hand, care givers and family members were ready to give up much more quickly.
As one of the posts on my blog discusses, it is difficult to know what might boost a person's hope or, conversely, to steal it away. People are so variable, and many behave much differently with the doctor than they do among their family and friends. Sometimes we get the wrong signals, and sometimes we send the wrong ones.
Perhaps I can learn some things from Dr Groopman that will help me to aim more accurately...
Having a diagnosis of incurable cancer changes you forever. Even if you are lucky to survive for years without treatment, you know without a doubt that you have an immediate threat to your life. If you get a bad cold, the flu, or stomach ailment, you start wondering if you will have to go to the hospital, if this is the end for you.
I think it's important to start tying up loose ends so that your heirs won't be left with a mess on their hands. Get the living trust or at least a will done, tell your relatives where you want to be buried, what kind of a service you want, maybe even write your own obituary.
Sounds morbid, but I suspect most of us have thought about leaving loved ones behind, and how to provide for them, the children, pets, parents, all of that. Instead of being downbeat and morbid, it is liberating, a few less things on their mind.
I'm still buying green bananas, but I'm not thinking of long-term retirement, that's for sure. I do want to have some time retired, but I really can't afford to retire now.
I'm thinking that when I need treatment, that's the time to leave work. Having treatment starts you down that final road. If you are lucky and actually respond to treatment (not all do, remember), you might have four or five years left. If you're lucky.
All of the hope in the world can't change the fact that you, we, are all going to die. That's life, folks.
I now make decisions in my life with its imminent end in sight. It's a fact. Make your peace with your Maker soon. It is a comfort.
I have scrolled through your review and having just finished the book,you left nothing out. Of course if you hadn't read the book you would not know that what you said is in the book. I loved the book, but I beleive you have spoiled it for new readers.
Sister Chemist
Post a Comment